Information for Patients
Heart disease is one of the leading causes of death in the UK. Quite often a patient will know what is wrong with them but not fully understand the condition. Sometimes you may not know what is wrong and will need tests carrying out so you know how to best manage your condition. Please take a look on our page at the most common conditions along with the tests used to diagnose these conditions. If at any point you would like to speak to someone about your cardiac condition please don’t hesitate to email through our contact page.
Conditions
- Angina & Chest Pain
-
Not all chest pain is due to angina. Angina, which means “strangulation”, is a symptom caused by the heart muscle being short of blood. It usually occurs when one or more of the coronary arteries which supply the heart with blood become narrowed or blocked. Typical angina occurs on effort such as walking quickly, running up the stairs or going up a hill, or may occur under emotional stress.
Angina or heart pain has specific features and the most important thing that a Cardiologist can do is to take an accurate history. Heart pain has certain specific features often being felt as a tightness or a heaviness in the chest rather than a pain, and often if feels as if someone has a heavy object sitting on the chest. It may radiate up into the jaw, the shoulders, the arms or the hands but not necessarily the left side. It may even be felt in the thumbs or the teeth. Often there are associated symptoms such as shortness of breath and sweating and also fatigue. Angina of effort is usually relieved by rest.
More severe forms of angina occur on minimal exertion or at rest and this is a medical emergency.
It follows that not all chest pain has a cardiac origin and chest pains of a different nature can be musculoskeletal, come from the stomach or gallbladder, or the lung.
The skill of the Cardiologist is to take an accurate history and come to a clinical judgement.
Sometimes it is absolutely clear from the history that the pain is or is not angina but there are many patients who have heart pain which doesn’t present quite so typically and again the skill of the Cardiologist is to tease this out and decide which tests are appropriate.
It is dangerous to mistake heart pain for indigestion.
- Heart Attack
-
A heart attack, properly known as a myocardial infarction, is a condition where part of the heart actually gets damaged because of shortage of blood. This may be due to a severe narrowing or even a total blockage of one of the coronary arteries and may occur out of the blue in someone who has previously never had any symptoms or in someone with previous angina.
The symptoms are usually much more dramatic than with angina and often produce severe chest pain or tightness, profuse sweating and shortness of breath.
The treatment of heart attacks has been revolutionised in the last few years by the development of what we call “primary angioplasty”. Now, instead of a patient with a suspected or proven heart attack being taken just to the nearest A & E Department, the ambulance service will transport the patient to the nearest Cardiac Centre that will supply a 24/7 service to take the patient directly to the Angio Lab, identify the blocked artery and open it up as quickly as possible, usually with the implantation of a stent.
The rationale for this is to restore blood flow down the blocked artery as soon as possible to stop the death of healthy heart muscle and its replacement by scar. Studies have shown that this is very successful in saving lives.
Nowadays a patient with a heart attack who is treated in this way may be discharged from hospital in 48-72 hours compared to 20 years ago where patients were kept in for a couple of weeks.
People may even be back at work within a week or so.
As with angina, some people fail to recognise their own symptoms of being a heart attack and erroneously treat themselves as having indigestion. Sometimes this is just due to denial.
Unfortunately some doctors make this error too, both with themselves and their patients.
Cardiologists would much rather see somebody with chest pains which turn out not be a heart attack than for people to delay seeing a doctor until it is too late.
If I had my way the word “indigestion” would be abolished from the dictionary!
- Palpitations & Blackouts
-
Palpitation is not really a diagnosis but is a symptom of an unusual awareness of ones heart beating. Many people have palpitations under conditions of anxiety such as taking an exam or a near miss in the car. Falling in love can have the same effect! Anxiety is very common and the body will pump out more adrenaline under conditions of anxiety leading to a stronger more obvious heart pounding as well as a faster heart rate.
Palpitations can also be felt when the heart changes rhythm and there are numerous disorders of the heart rhythm. The most common ones are ectopic beats from the upper or lower chambers of the heart. Any piece of the heart muscle is capable of putting in an abnormal beat a bit like a rogue violinist in a orchestra playing a note at the wrong time. This may be felt as an extra beat or even a skipped beat. After these extra beats there is a pause while the heart resets itself and this may produce a sinking feeling.
Normally in people with healthy hearts ectopics beats are totally benign but they can be a real nuisance. You don’t have to have anything actually wrong with your heart to experience ectopics and most people will get them at sometime or another.
Fatigue, jet lag, too much alcohol, coffee or tea, lack of sleep, stress or flu-like illness are just some of the things which can increase ectopics. They are often cyclical and may bother you for a few weeks and then disappear.
Symptoms are very subjective. Some people may have only a few ectopics in a day and feel totally unable to function whereas others may have several thousand and not notice any of them.
Sometimes ectopics accompany mild or serious forms of heart disease and the Cardiologist will be able to tell you whether yours are benign or not, and whether or not they need some treatment.
Another very common rhythm disorder is a called atrial fibrillation and this will probably be the single most common rhythm disorder which Cardiologists see. There are a variety of causes including high blood pressure, diseases of the heart muscle, an overactive thyroid or even acute illnesses such as pneumonia.
In this condition the upper chambers known as the atria don’t actually beat but shiver and shake at a very fast rate making the lower pumping chambers beat rapidly and irregularly.
Again some people don’t know they have got it but others will experience rapid palpitations, and may feel dizzy or unwell or even experience breathlessness or chest pain.
There are many investigations for atrial fibrillation and many forms of treatment. The single most important thing with atrial fibrillation is to prevent strokes because clots can form in the upper chambers of the heart break off and get stuck in the brain. Sometimes it is necessary to give formal anticoagulation with Warfarin or one of the newer drugs which are becoming available which are Warfarin substitutes.
There are many other forms of rhythm disorder that can occur including those due to abnormal electrical connections in the heart, and more serious ones from the lower chambers of the heart. The Cardiologist will be able to detect these with various tools available to us and advise on the best treatment.
Blackouts may or may not have a cardiac origin. There are numerous cardiac causes including the heart going too slowly which is known as a bradycardia, the heart going too fast which is known as a tachycardia or other conditions such as a vasovagal attack often produced when a pulse and blood pressure drop, but there are other conditions which can cause blackouts including neurological ones or blood clots on the lungs for example.
Generally speaking with slow heart rates, if the heart does beat too slowly due to an electrical fault this can be remedied with a Pacemaker.
Fast heart rhythms may require drugs or even electrical procedures know as ablations.
The most severe form of fast rhythm disorder where the heart shivers and shakes and goes into something called ventricular tachycardia or ventricular fibrillation may require the implantation of a defibrillator to apply an electric shock to restore heart rhythm.
- Breathing Difficulties
-
Breathlessness has a variety of causes not all cardiac. Being overweight or unfit or having dodgy knees or hips can produce breathlessness.
Breathlessness from the heart may indicate a form of heart muscle disease such as a damaged heart due to a heart attack, or a disease or a primary disease of the heart muscle. Breathlessness may occur as part of angina when the heart is short of blood.
The Cardiologist will be able to tell whether the heart is the primary cause of the breathlessness or whether there is another cause as above or as is so common these days, whether the breathlessness comes from the lungs due to for example smoking related diseases.
Tests such as an echocardiogram would be an important part of deciding whether someone’s breathlessness is caused by the heart.
Tests
- Electrocardiogram
-
The electrocardiogram ECG is a very simple and widely available heart beat trace where the electrical activity of the heart is produced on paper as a serious of wiggly lines. It is a low technology test and by no means tells us everything about the heart. The ECG may show evidence of enlargement of some of the cardiac chambers, electrical faults and some rhythm disorders. It is important to realise the limitations of the ECG. For example, a normal ECG does not in anyway exclude possible underlying disease of the heart arteries. An ECG carried out during chest pain may show changes of the heart being short of blood and absolutely vital in the presence of an acute heart attack.
- Exercise ECG
-
The exercise ECG records the heart beat under physical stress, and its main use is to try and detect whether the heart maybe short of blood during exercise. There are certain changes which may occur in the electrocardiogram during exercise if and when the heart becomes short of blood. The changes may not be apparent until one actually stops exercising ie. during the recovery period.
The exercise test is not the most sensitive or specific test in the world. Unfortunately it is often used as part of screening or for mortgage or life insurance applications. Although actuaries in the insurance companies are keen on this, Cardiologists have long recognised the limitations of the exercise ECG as part of screening in well people. People may be misleadingly reassured but equally commonly, the exercise stress test may produce abnormalities that are “false positives” and lead to further unnecessary investigations and a lot of anxiety.
The bodies such as the America College of Cardiology do not recommend the use of stress tests as part of a well person screen.
Other reasons for doing the exercise ECG maybe to look for rhythm disorders and to gauge the success of treatment.
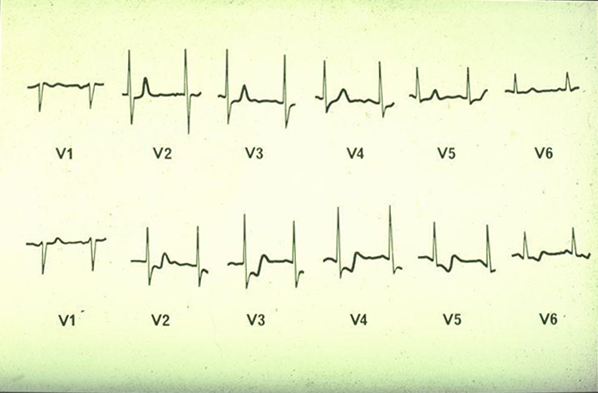
Traces from an exercise ECG showing abnormalities of the traces during exercise unmasking shortage of blood from heart muscle. - The Chest X-Ray
-
Like the ECG the chest x-ray is widely available and simple. Some limited information can be gleaned from a chest x-ray including the size of the heart (although not the individual chambers), the width of the aorta which is the main artery coming out of the heart and the lung fields can be assessed to see if they are clear, congested, infected or have any fluid in their lining.
- The Echocardiogram
-
The echocardiogram or cardiac ultrasound is now a cornerstone of heart imaging. It is essentially the same test that pregnant women have to look at the baby in the womb. The echocardiogram produces moving pictures on a screen of the heart muscle, the valves and the chambers. A huge amount of information can be obtained from a cardiac echo including whether the each of the heart chambers is the normal size, whether the heart muscle is too thick or whether there is any evidence of scarring and whether any of the heart valves are leaking or narrowed. It is also possible to assess how bad the narrowing or leaks are.
The echo is also used to assess the lining of the heart and see if there is any fluid there.
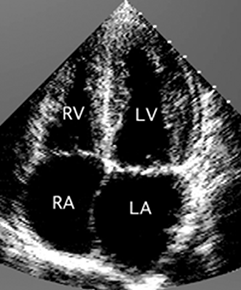
Echocardiogram or ultrasound of the normal heart showing all 4 chambers 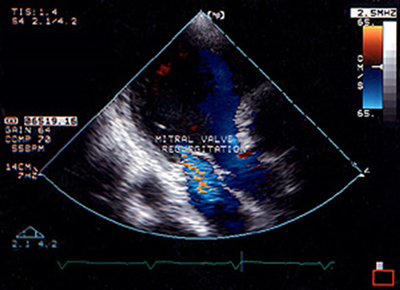
Echocardiogram using the Doppler technique to show a leaking mitral valve. 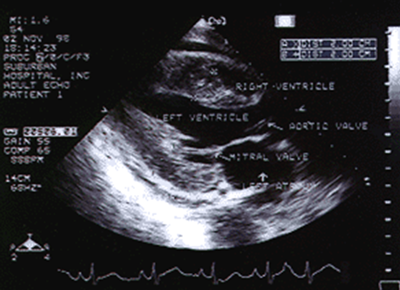
Echocardiogram showing very thickened heart muscle in hypertrophic cardiomyopathy. 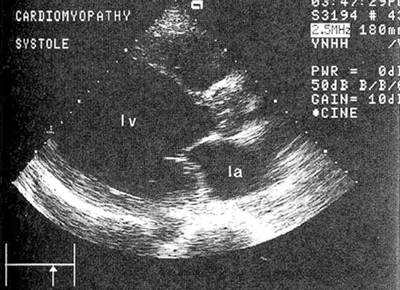
Echocardiogram showing a very enlarged and damaged left ventricle. - Transoesophageal Echocardiogram
-
This is a slightly more sophisticated form of the echo where instead of the probe being placed on the chest wall, a small probe is actually swallowed and the heart imaged from the gullet. The reason this is useful is that some of the back parts of the heart are very close to the gullet and ultrasound images from the gullet produce better quality pictures of the mitral valve for example and the left atrium. It is possible to see if there are any clots in the left atrium.

Transoesophageal echo (swallowing echo or TOE) showing clear pictures of the left atrium, mitral valve and left ventricle - Contrast Echocardiogram
-
This involves injecting some agitated saline into a vein in the arm and looking to see if micro bubbles pass from one side of the heart to the other. This is done to look for a hole in the heart particularly something called a PFO or patent foramen ovale. Normally there is a structure called the septum which separates the right side of the heart from the left side of the heart but if there is a small defect here then we can see the passage of bubbles during the echo. This has relevance in people who have unexplained strokes for example.
- Nuclear Imaging
-
Radioisotope imaging has been used to assess the heart for more than 30 years. The most commonly used form is what we called perfusion imaging which is a more sophisticated and accurate form of the exercise test. Perfusion imaging allows coloured pictures to be produced which match the blood flow into the heart muscle. It follows that if we stress the heart either by exercise on a bicycle or treadmill, or more commonly now during this test with drugs to open up the heart arteries, then if we image the heart when it is stressed and again when the heart is at rest any abnormalities of flow will appear as differences in the colour pictures between the two sets of images. This is widely used in Cardiology and incredibly valuable to detect “inducible ischaemia” ie. whether the heart becomes short of blood under stress even though it not be at rest.
This test is often used to decide whether someone should have an angiogram or not or even can be used after the angiogram to decide whether an artery needs to be treated with an intervention or not.
The amount of radiation exposure is extremely small and the test is very safe.
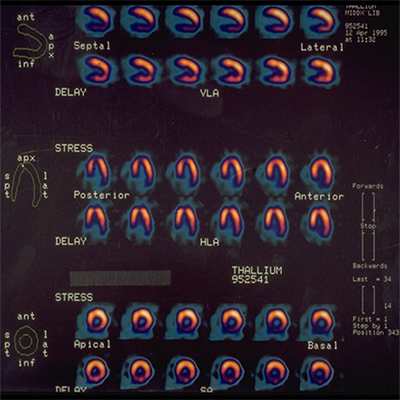
Images from a radio-isotope (nuclear) perfusion scan comparing rest and stress images of the heart in different views showing blood flow. 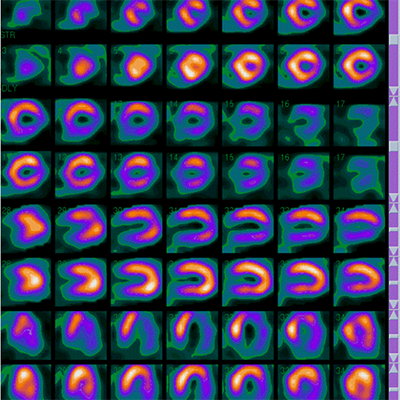
Severely abnormal radioactive heart scan in a patient with no symptoms who had three blocked arteries and underwent bypass surgery urgently. - Cardiac Screening
-
This is an area that has changed greatly in recent years. Recognising those at risk from various forms of heart disease enables preventative measures to be taken, whether it is life style changes or medication, before the disease presents with a life threatening illness.
Certain tests are used depending on what we are looking for. In elite athletes for example, we screen for inherited diseases of the heart muscle or the electrical tissue in the heart, that might only cause problems under extreme exertion.
In the larger population, screening looks for arterial disease, particularly of the coronary arteries in the heart to detect the earliest signs and hopefully therefore to prevent heart attacks and deaths in the future. It is not possible to screen everybody but the skill is to identify those people who need a careful look with modern technology and ensure they receive the right advice and/or medication.
Many people with high cholesterol levels but no other risk factors are prescribed medication to lower cholesterol ,and sometimes as a result of the appropriate tests, we can discontinue these medications.
Looking for chalky deposits in the walls of the arteries enables us to see if someone does have the earliest signs of furring up, and the Calcium Score is a simple CT X-ray, which gives a more individual assessment of risk than the tables that are widely used. A normal score confers low risk, and the higher the score, the higher the risk and the more aggressive the prevention needed.
Examples of Coronary Artery Scans
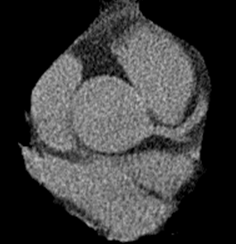
No calcification 
Moderate calcification 
Significant calcification 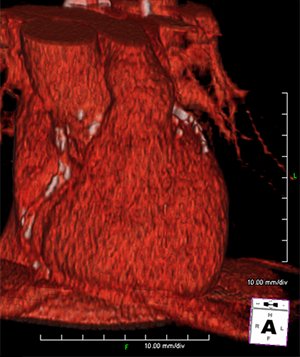
Image from a coronary calcium scan showing extensive calcification in the hearts arteries. The score was 3400. - Cardiac Magnetic Resonance
-
This is the latest addition to our armoury. Cardiac MRI produces high quality pictures and is used in a whole variety of conditions. It can be used to detect specific disorders of the heart muscle, to assess the valves, and now it can also be used an alternative to the radioisotope test to look at heart blood flow. The main limitation of MRI is that it is not widely available yet as some other tests and some people who are very claustrophobic are unable to go into the machine.
The MRI scan often gives us information not obtainable by any other means.
- Cardiac CT
-
This is another area which has revolutionised the practice of Cardiology. There are many uses of cardiac CT and historically it has often been used to diagnose tears called dissections in the aortic wall, to assess other forms of aneurysms, and to look at the lining of the heart.
More recently CT is now able to produce high quality non-invasive angiograms which are pictures of the coronary arteries. Until the development of fast cardiac CT, the only way we could look at the coronary arteries is to do a formal invasive angiogram (see below).
There are now CT scanners with more than 600 slices which can produce high resolution pictures of the coronary arteries and identify whether they are normal, or whether there are any deposits of calcium or chalk in the walls or whether there are any major narrowings.
The National Institute of Clinical Excellence for Health (NICE) has produced guidelines which recommend the use of cardiac CT as an alternative to other tests such as the nuclear scan or the invasive angiogram and certainly in the Private sector this test is now widely available and has totally revolutionised the management of patients with chest pain.
The CT can also tell us whether there is what we call soft plaque in the arteries which is the plaque which is the vulnerable type of plaque that may clot off and cause heart attacks.
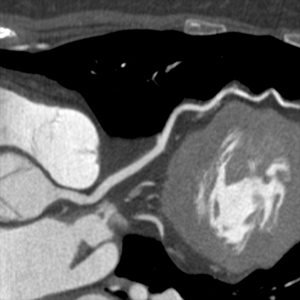
Normal left anterior descending on CT 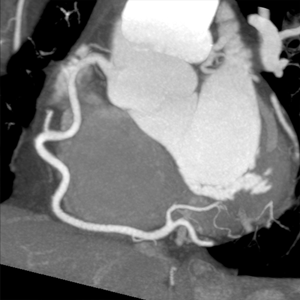
Normal right coronary artery on CT 
Normal circumflex artery on CT 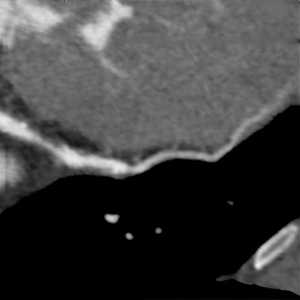
Significant soft plaque in LAD artery on CT - 24-hour Monitoring
-
Both blood pressure and heart rhythm can be monitored for 24 hours by attaching you to a small device in the case of a rhythm monitor or a blood pressure cuff. 24-hour monitoring is very useful for detecting rhythm disorders that don’t happen to manifest themselves when you are actually with the patient. It is useful for both diagnosing and ruling out serious arrhythmias.
For the 24-hour rhythm readings to be useful, the Cardiologist must first establish that there is likely to be yield of picking something up in those 24-hours. It is not therefore useful if someone have their symptoms only once a fortnight. More prolonged periods of monitoring may be necessary under those circumstances.
24-hour blood pressure monitoring is really useful particularly for people who have high blood pressure when they come to see a doctor! This is often called the “white coat syndrome” and it is amazing how people can have really high readings in the presence of a doctor and yet half an hour later they are back to normal.
The 24-hour blood pressure monitor enables us to see whether someone really does have high blood pressure or has the white coat syndrome and either start treatment or advise against it.
Some people find that wearing the blood pressure cuff quite uncomfortable because it pumps your arm up several times during the day and night but it is invaluable for your Cardiologist.
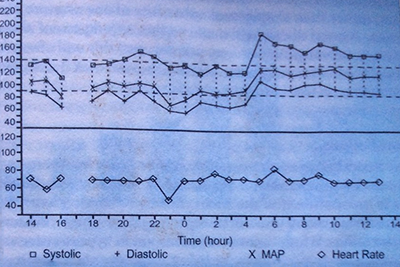
24 hour blood pressure recording in a patient with a recent small stroke, showing early morning surge in blood pressure at around 5 am. - Reveal Device
-
The Reveal Device is your own personal implantable monitor and this device is recommended in people who have symptoms such as palpitations or blackouts too widely spaced apart to catch on conventional monitoring. The device looks like a small cigarette lighter and it takes about 15 minutes to pop it under the skin as a day case in hospital. It can stay in for up to two years and records every single heart beat at that time. It can be asked to look for fast or slow heart rates and the patient has a little device to activate it when he/she feels unwell. The traces can then be retrieved by the Cardiac Department.
Many people have been found to have quite serious rhythm disorders or even to need heart pacemakers based upon the findings of the Reveal Device.
- Coronary Angiography
-
This forms part of the investigation known as cardiac catheterisation and is where the Cardiologist places a small catheter actually inside the patient’s circulation. This is done in a dedicated operation suite known as a Catheter Lab or an Angio Lab.
Angiography is performed under a local anaesthetic often with a little bit of sedation and is carried out either through the large artery in the skin crease in the groin known as the femoral artery or frequently nowadays via the radial artery at the wrist.
A small tube known as a catheter is passed under x-ray control from one of these arteries into the heart and a specially shaped catheter is put gently into the orifice of the coronary arteries and iodine containing contrast medium (commonly known as dye) is injected gently down the arteries and filmed on digital x-ray material.
The passage of the contrast medium will identify any narrowings or blockages throughout the coronary tree.
It is also possible to take a film of the left ventricle and the aorta at the same time as well as measuring all the pressures in the various heart chambers.
Although the test is invasive it is incredibly safe in experienced hands and the complication rates are very very small.
Nowadays, as above, CT angiography can replace invasive angiography especially when the Cardiologist thinks that the arteries are going to be normal.
An invasive angiogram would be used instead of a CT if the Cardiologist thinks it is highly likely that someone’s symptoms are due to angina, or if someone has had a definite or suspected heart attack.
- Coronary Intervention or PCI
-
Treating blocked or narrowed coronary arteries with balloon angioplasty or stenting has now been around for 30 years. In this procedure, after taking pictures of the arteries with the angiogram, a serious of guide wires, balloons and stents are passed into the area of the artery which is narrowed or blocked and the balloon and stent are used to squash the blocking material out of the way and to scaffold the artery and re-establish flow.
The main indication for this is for people with angina but it is also now carried out in patients who have an acute heart attack. There are many forms of balloon and stents available but nowadays the most common form of stents are medicated or drug eluting. These have a special medicine on the coat of the metal part of the stent, the metal being delivered into the wall of the artery to prevent re-narrowing and this revolutionised this treatment.
It is possible to treat more than one artery with stenting but the Cardiologist will decide at a certain point when and if there are too many narrowings to be treated appropriately by stenting and whether bypass surgery should be carried out.
Because stents have been so widely publicised and most people know about them, patients tend to prefer to have stents than bypass surgery. This is because the procedure is done via the wrist or the groin under local anaesthetic and may only involve one night in hospital. Conversely a bypass operation is a three to four hour operation with 7-10 days in hospital.
However the Cardiologist must be certain that stenting is the right procedure and there are many research papers which have highlighted where and when stenting is appropriate but also where bypass surgery has better results.
Narrowings of the left main stem artery for example are usually best treated with surgery under most if not all circumstances.
Patients who have had bypass surgery who develop narrowings in their bypasses can also be successfully treated with stents in the bypasses to keep them open and prolong their life.
Until recently longstanding total blockages of coronary arteries have not been successfully treatable by stenting. However this is changing as the technology improves and it is now possible to reopen arteries which have been blocked for many years in many cases.

Angiogram of a blocked right coronary artery in a heart attack patient 
Artery after the clot has been removed by a special catheter (the dye now flows beyond the blockage) 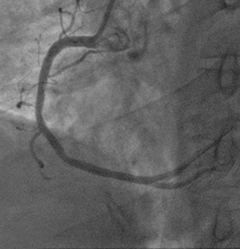
Artery after it has been stented over the blocked segment where the clot was 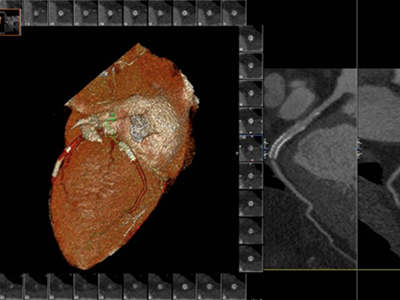
Patent stents in RCA on CT - Open Heart Surgery
-
Open heart surgery is used to bypass the coronary arteries and/or to change a heart valve which is diseased. Coronary artery bypass surgery is nowadays reserved for those people who cannot be treated by angioplasty or stenting because the disease is too advanced.
In most cases the left internal mammary artery is used to bypass the artery down the front of the heart. This artery known as the LIMA is already present in the chest and supplies breast tissue and some of the muscles and the skin of the chest wall. Because it is also an artery, when it is used as a bypass for the artery down the front of the heart the results have been spectacularly good and it may well stay open for 25-30 years.
Other arteries in the heart are bypassed using veins from the leg known as the saphenous veins. This is a very successful operation although the survival of these venous bypass grafts is not as good as the survival of the internal mammary.
Nevertheless, nowadays many patients can expect 15-20 years of good health from their bypass operation particularly with avoidance of smoking and adequate treatment of high cholesterol etc.
- Heart Valve Replacements
-
Narrowed or leaking heart valves need to be replaced. The valve used may either be a tissue valve or a metal valve depending upon various factors such as the need to avoid form anticoagulation with Warfarin, whether a patient is of childbearing age or not as well as patient preference.
- Aortic Valve Stenting (TAVI)
-
Many patients nowadays can be treated with a TAVI which is where the aortic valve is replaced without open heart surgery using an aortic valve stent.
This has not yet become applied to everybody and is currently mainly used for people who have severe narrowing of the aortic valve who are considered not fit enough to have an open heart operation. This maybe because of age, frailty, poor lungs or poor kidneys where the risks of going onto a heart bypass machine are considered too high.
Aortic valve stenting is now being successfully used and no doubt with develop more in the years to come and be more widely applicable.